

Physicians are often reluctant to prescribe opioids for patients with chronic pain despite initiatives to promote evaluation and treatment and even the development of national pain management guidelines. 1 Among their concerns are the potential for patient addiction, medication tolerance, physical dependence, and the possibility of abuse, misuse, or diversion of opioid medications. This last area is a growing problem as 4.9 million people 12 years or older were nonmedical users of pain relievers in 2012, and the growth rate of new nonmedical users of pain medication is second only to marijuana. 2 Concerns about patient safety and the potential for regulatory sanctions led to growing interest in discontinuing chronic opioid therapy prescribing in our 24-provider urban family medicine clinic, which is affiliated with the University of Michigan Health System's Department of Family Medicine. The clinic team agreed that creating a controlled substance policy was in order. Establishing policy and procedures would minimize differences between individual providers' approaches to chronic pain management and the associated confusion that we feared made it easier for misuse and abuse to fly under the radar. We also believed it would enhance our ability to educate resident physicians about chronic pain management.
A work group of staff from all five of the department's community-based family medicine clinics began developing an opioid monitoring process for eventual use department-wide. This article describes the components of our systematic, patient-centered approach for treating patients with chronic pain, which can be adopted in other primary care settings.
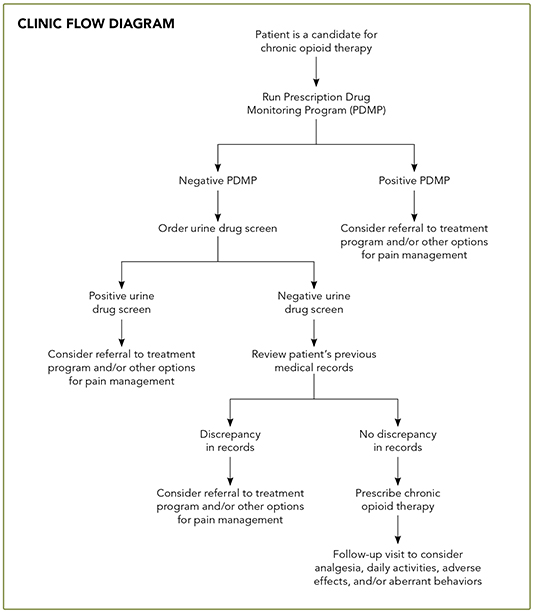
We follow a multi-step process for evaluating any patient considered a candidate for chronic opioid therapy. (See “Clinic flow diagram.”) The patient is given a copy of our policies for treating chronic pain and prescribing opioid medication and a controlled substance agreement, which he or she must sign. In addition, we obtain a urine drug screen and a report from the state of Michigan listing what controlled substances, if any, have been prescribed for the patient within the past year. It is also our policy that new patients must provide medical records from previous doctors. Once we have received and reviewed the patient's lab work, report, and medical records, we are able to make an informed decision as to whether a patient is eligible to receive chronic opioid therapy in our office.
Our Chronic Pain and Opioid Medication Policies were developed by a committee that included at least one physician champion per site as well as various other staff members, including clinic managers, nurses, and medical assistants. The committee garnered input from clinic staff and administrators in establishing policies designed to foster a therapeutic physician-patient relationship and reduce stress for clinical staff.
The document states that most patients will need to come in for a visit every one to three months, although the frequency of visits is ultimately at the discretion of the physician. In addition, we stipulate that prescriptions are written to last until the next office visit and refills are generally not provided over the phone unless pre-arranged and documented by a physician in the medical record. The document also states that lost or stolen prescriptions or medications are not replaced and that we expect patients to comply with other recommended medical treatments, including consultations and imaging studies. Patients are given a hard copy of these policies to review annually.
The University of Michigan Health System has its own set of chronic pain guidelines, which serve as an adjunctive resource for managing patients who receive chronic opioid therapy. The guidelines include several helpful tools, such as a sample controlled substance agreement and clinic policy in addition to a selected medication table that includes dosages and cost information. The appendices attached to the university's guidelines provide several helpful tables to guide opioid discontinuance and assess opioid risk.
Before your doctor first decides to prescribe opioid pain medications for you, we will need medical records from your previous doctors and a urine drug screen. We will also obtain a report from the state that shows which controlled substances, if any, have been prescribed for you in the past year. We require these items in order to make good decisions about your treatment.
Please note that at least once a year you will need to provide a urine sample. We will also obtain a report from the state, at least once yearly, that outlines the prescriptions you have received from pharmacies.
As part of your opioid treatment plan, we will require that you sign a controlled substance agreement once a year. Please read this agreement carefully, as it has useful and detailed information that is not discussed in this policy letter.
To provide you with the best possible care, we will need to monitor your prescriptions. This will be done during scheduled office visits. Most patients will need to be seen at least every one to three months.
Your prescriptions will be written to last until your next visit. If you have a problem with your condition between office visits, you should schedule an office visit with your health care provider at that time. Please note that opioid prescription refills will not be given over the phone unless you have arranged this ahead of time with your doctor. Any medications that are lost or stolen will not be replaced.
Additionally, you will be expected to use other medical treatments to improve your pain. It may not be possible to completely remove all of your pain. However, our goal in many cases is to return your functionality to an accepted level. Your health care team is able to provide the best treatment for you if we have good communication. You and your health care providers should be respectful of each other for treatment to continue.
YOUR RESPONSIBILITIES